LEADING ARTICLE
Renoprotection – a system of measures primarily pharmacological control, contributing to the continued preservation of renal function. Any medical activity or medicines that lead to a slowdown, suspension or reversion of eGFR could be considered as renoprotective. Currently, renoprotective drugs with evidence-based efficacy include angiotensin-converting enzyme inhibitors (ACEIs), and recently SGLT2 inhibitors. It is known that the therapeutic efficacy of renoprotective drugs depends on the initial eGFR. Hence, choosing renoprotection medicines, it is necessary to consider not only the estimated GFR (using the EPI formula), but also a functional renal reserve. Physiologically sound is the method of determining the renal reserve with oral administration of 0.45-0.50% sodium chloride solution at the rate of 0.5% of body weight. The definition of a renal reserve based on this technique, as a routine method for examining nephrological patients, provides additional information not only on the number of functioning nephrons, but also on their condition. Based on a retrospective analysis of more than 15 years of using ACEIs and studying the functional renal reserve, we proposed a differentiated approach to the appointment of renoprotective medicines in mono regime or drugs combination, taking into account the stage of the disease and the functional renal reserve for maximum preservation of functioning nephrons. This approach has been used by us for the past three years in clinical practice.
REVIEWS AND LECTURES
Interest in studying the role of the gastrointestinal tract in maintaining homeostasis in chronic kidney disease is a traditional one. It served, in particular, as a starting point for the creation of enterosorbents. However, if earlier the main attention was paid to the mechanical removal of a number of potentially dangerous biologically active substances, recently an intestinal microbiota has become an object of interest. The first part of the review of the literature on this topic is devoted to questions of terminology, the normal physiology of the colon microbiota. A detailed description of dysbiosis is given. The features of the main groups of microorganisms are reflected. The hypothetical and confirmed interrelations of the intestine-kidney axis are presented. The pathogenetic mechanisms of the influence of colon dysbiosis on the processes of local and systemic inflammation are discussed. The influence of dysbiosis on the state of the kidney parenchyma and its participation in the progression of CKD are debated.
To date, the expression of both the “olfactory” receptors (OR) themselves and the components of the olfactory signaling system, «olfactory» adenylate cyclase (AC3) and “olfactory” G protein (Golf), has been found in various structural and functional parts of the kidney. In the human kidney, at least 13 genes of various “olfactory” receptors are expressed, excluding pseudogenes. Olfr 78, Gpr41, Gpr43, OR51E1, OR11H7 “olfactory” receptors have been found to play a role in the regulation of blood pressure in response to changes in the blood concentration of short-chain fatty acids, mostly produced by intestinal microbiota. The role of AC3 and G olf in renin secretion, control of SCF and obesity predisposition is shown. Olfr1393 “olfactory” receptor is supposed to be involved in glucose reabsorption in the proximal tubule of the kidney due to functional modulation of sodium glucose cotransporter Sglt1 responsible to 3–10 % glucose reabsorption in proximal tubule. Hypotheses on the relationship of “olfactory” signaling component defects with the development of pathological syndromes, such as kidney diseases, different types of ciliopathy (Bardet–Biedl, Joubert, Meckel syndromes) and valproate administration associated Fanconi syndrome, are given. The study of “olfactory” signaling components in the structure of the kidney, as well as their role, both in physiological functions and in the development of renal pathology, creates a scientific basis that will be useful not only for nephrologists and pharmacologists, but also for clinicians of other specialties from the point of view of developing new pharmacological approaches in order to target the detected defects.
Arterial hypertension (AH) resistant to drug therapy is the phenotype of uncontrolled AH, in which patients receiving at least 3 antihypertensive drugs, including a diuretic, maintain blood pressure above the target level. Initially, the term refractory hypertension was also used to refer to resistant hypertension. Recently, however, refractory hypertension has been isolated into a separate phenotype of difficult to treat hypertension, which is defined as insufficient control of target blood pressure, despite the use of at least 5 different mechanisms of antihypertensive drugs, including long-acting diuretic and antagonist of mineralcorticoid receptors. Resistant hypertension is detected in 10–15 % of all hypertensive patients receiving drug therapy, and is often found in patients with chronic kidney disease. Hypertension can be a cause and/or consequence of kidney damage and is typical of most patients with chronic kidney disease. The lack of control of target blood pressure in a significant proportion of hypertensive patients with CKD who receive at least 3 antihypertensive drugs of different mechanisms of action indicates a lack of effectiveness of antihypertensive therapy, which not only accelerates the loss of renal function, but also significantly worsens the prognosis, contributing to such people risk of cardiovascular and renal complications. The review presents data on the prevalence, prognostic value of resistant hypertension in patients with chronic kidney disease, features of its formation and approaches to increasing the effectiveness of antihypertensive therapy in this patient population.
ORIGINAL ARTICLES. CLINICAL INVESTIGATIONS
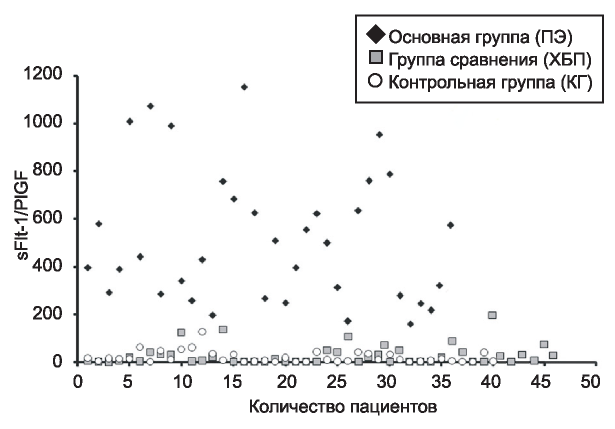
THE AIM: To assess the significance of prognostic markers of preeclampsia – sFlt-1 and PlGF in the differential diagnosis of preeclampsia and chronic kidney disease. PATIENTS AND METHODS: patients whom signed informed consent, was taken samples of blood in the third trimester of pregnancy. The study group included 36 patients with preeclampsia, the comparison group of 46 pregnant women with CKD and the control group included 40 healthy patients, with pregnancy without complication. RESULTS: Significant differences in the levels of serum sFlt-1 and PlGF were found: between the PE and the comparison group (CKD), as well as between the PE and the control group (CG), whereas no differences were found between the CG and CKD. The sFlt-1 level was significantly increased in PE compared with CKD and KG (5.12-fold and 4.25-fold higher, respectively). Serum PlGF levels were significantly reduced in PE relative to both CKD and KG (17.4 and 12.5 times lower, respectively). The sFlt-1/PlGF ratio was significantly increased in PE compared with CKD and the control group (approximately 25 times higher in both groups), but there was no significant difference between CKD and CG. CONCLUSION: Thus, the definition of the relationship sFlt-1, PlGF, sFlt-1/PlGF can be used in the differential diagnosis of preeclampsia and chronic kidney disease.
Fabry disease (FD) is a progressive multi-organ disease leading to the development of cardiovascular and cerebrovascular complications and progression of renal failure. Nonspecificity of clinical signs often leads to late diagnosis of the FD that causes high diagnostic relevance of screening in high risk groups, particularly among patients with chronic kidney disease (CKD). According to the results of screening programs in many countries, the average prevalence of FD among patients with CKD is about 0.26%. THE AIM of this study was to investigate the prevalence of FD in patients with CKD in the northern west region of Russian Federation. PATIENTS AND METHODS. This prospective study assessed α-galactosidase A (α-Gal A) activity in dried blood spots in 1835 stage 1-5 CKD (85% – dialysis, 15% – pre-dialysis) patients, 74% males, mean age 55±12 years. The survey was carried out regardless of gender, age and primary diagnosis leading to CKD. The activity of α-Gal A more than 1.89 umol/l/hr was considered as normal. In the case of identifying the decreased activity of the enzyme the diagnosis was confirmed by GLA gene mutation analysis. RESULTS. The average level of α-Gal A was 5.39±2.69 umol/l/h. The level of α-Gal A was significantly higher in patients with pre-dialysis stages of CKD compared with patients receiving dialysis (7.5±3 vs 4.3±2.3 umol/l/h, p<0.001) as well as in males higher than in females (5.9±3.4 vs 3.4±2.3 umol/l/h, p <0.001). The decrease in α-Gal A activity was detected in 6 patients, of which 3 had the GLA gene mutations (c.427G>A, с.818Т>С, c.895G>C). One patient (p.508G> T) had a confirmed FD and received an enzyme-replacement therapy at the time of screening. All patients with identified FD were males treated by hemodialysis. Thus, the prevalence of FD in patients with CKD C5d was 1:392 (0.26%). A survey of relatives revealed the disease in two additional cases. CONCLUSION. The prevalence of Fabry disease in selected CKD patients of northern west region of Russian Federation is in the mean worldwide range. In all cases, the FD was not timely diagnosed, leading to serious organ damage and delaying the onset of enzyme replacement therapy. Thus, the screening of FD is necessary at the early stages of CKD.
It is known that patients with chronic kidney disease (CKD) often have hypothyroidism. In patients with CKD, iodine excretion in the urine is disrupted. The high content of iodine in the thyroid gland and tissues leads to a disruption in the synthesis and peripheral metabolism of thyroid hormones. In hypothyroidism, there is a disruption of sodium and water reabsorption in the proximal tubule, the volume of the filtrate increases, the volume of the tubular apparatus overloads, and the eGFR decreases. THЕ AIM: to study the occurrence of hypothyroidism in patients with different stages of CKD, to evaluate the parameters of thyroid status and antithyroid antibodies in patients with CKD. PATIENTS AND METHODS. 953 patients from I.P. Pavlov SPbSMU clinics (screening group) were examined. TSH, free T4, serum creatinine were defined and eGFR was calculated using the formula CKD-EPI in all patients. A group of patients with hypothyroidism accounted for 466 patients. Patients with a normal TSH of 0.4-2.5 mIU / L (comparison group) were selected from the screening group. RESULTS. eGFR in the screening group and in the group of hypothyroid patients correlated with age. Hypothyroidism was associated with female sex and older age. In the group of patients with advanced stage CKD (3B-5), the incidence of subclinical and manifest hypothyroidism was 3 times higher than in the group with normal GFR (GFR> 90 ml / min, p = 0.007). In the group of patients with hypothyroidism, the frequency of advanced stages of CKD (3B-5) was 2 times higher than in the comparison group (p = 0.02). In patients with CKD, a direct correlation was found between GFR and free T3 (r = 0.34, p = 0.02). Thyroid peroxidase antibodies were revealed in 64% of patients with CKD with hypothyroidism. CONCLUSION. Hypothyroidism is associated with chronic kidney disease. For patients with CKD, there is a syndrome of euthyroid pathology ("low T3" syndrome). Hypothyroidism in patients with CKD is not always the outcome of autoimmune thyroiditis.
Selective vitamin D receptors agonist paricalcitol can increase probability of proteinuria reduction at patients with the chronic kidney disease (CKD) and secondary hyperparathyroid-ism. THE AIM of this study was to determine the cost effectiveness of oral paricalcitol in patients with a CKD and secondary hyperparathyroidism and to carry out the budget impact analysis to understand the potential financial effect of introducing this drug in a health plan. MATERIALS AND METHODS. Assessment was carried out from a health care payer per-spective with use of the 5-year temporary horizon. Markov modeling on the basis of results of double blind trials at whom the efficacy of a paricalcitol at patients with hyperparathyroidism was estimated is carried out. The analysis is carried out taking into account tariffs of compulsory health insurances across St. Petersburg for 2018. Cost of paricalcitol corresponded to the price of registration including VAT for 2018 and 10% of a trade extra charge (5061.27 rub for 28 caps. on 1 mcg). During cost-effectiveness assessment clinical and economic outcomes were discounted at 3,5% a year. The budget impact analysis was carried out without discount-ing. RESULTS. Purpose of an oral paricalcitol to patients with CKD stage 3-4 and secondary hyperparathyroidism allows to increase time before transition to dialysis and life expectancy on average for 0,049-0,134 and for 0,033-0,144 year, respectively (when calculating without dis-counting). The cost effectiveness of an oral paricalcitol is higher at early stages of a nephropathy – 1,377 million rubles / year without dialysis gained, 1,408 million rubles / life year gained and 1,647 million rubles / QALY. At the same time paricalcitol therapy of patients with early stages of a nephropathy demands increase of cumulative expenses in 5 years by 2,24 times. CONCLUSIONS. Oral paricalcitol therapy in patients with a CKD and secondary hyperparathyroidism, according to results of modeling, allows to postpone transition of patients to dial-ysis and, taking into account the made assumptions, can be considered in patients with early stages of a nephropathy as economically acceptable intervention.
THE AIM: to assess the effect of ubiquitin-independent protein degradation on the development of protein metabolism disorders in patients with CKD who are treated with hemodialysis. PATIENTS AND METHODS: 80 patients with CKD treated with hemodialysis were examined. The study group included: 47 men and 33 women, whose average age was 51.7 ± 11.6 years, the duration of dialysis were 33.5 (0.5; 236) months. An anthropometric study, bioimpedancemetry, determination of muscle strength, biochemical blood analysis and an open ELISA for the presence of a 20S proteasome (20S-PSM) in the blood were carried out to all patients. RESULTS: When building regression analysis models, age, duration of dialysis, serum albumin, 20S proteasomes had a significant effect on muscle strength. There was no statistically significant correlation between the level of 20S-PSM and serum albumin and total protein as an independent result of proteasome protein degradation (p = 0.78; p = 0.80). CONCLUSION: The study demonstrated the relationship of the level of 20S proteasome with the features of dialysis treatment, the level of chronic inflammation. The change in body composition in the form of a compensatory increase in the absolute content of adipose tissue on the background of sarcopenia was not revealed according to the results of bio-impedance, which requires further study.
ORIGINAL ARTICLES. EXPERIMENTAL INVESTIGATION
THE AIM. To study the renal function of rats in conditions of streptozotocin-induced model of experimental diabetes mellitus. MATERIAL AND METHODS. The study was conducted on 25 male Wistar stock rats (12 individuals – a group of intact rats and 13 individuals – a disease control group). Diabetes mellitus was simulated by intraperitoneal administration of Stretpozotocin at a dose of 65 mg / kg. For a more selective simulation of type II diabetes, rats of the disease control group were injected intraperitoneally with a cytoflavin solution at the rate of 115 mg / kg nicotinamide dosage. In both groups, the daily urine volume was collected every 7 days during the month, in which the concentrations of glucose, protein, and creatinine were determined. Taking into account the daily volume of diuresis, excretion of glucose, protein, and creatinine was calculated. RESULTS. At baseline, all determinable indicators of renal function in rats did not differ between groups. Then, in the disease control group, there was a significant increase in daily diuresis, protein excretion, glucose excretion, and creatinine. As a result, by the end of the experiment, the magnitude of these indicators exceeded the level of intact rats by 2.0; 1.5, 3.2 and 1.9 times, respectively, CONCLUSION. Under conditions of the streptozotocin model of diabetes mellitus, characteristic changes in the renal excretory function are observed: an increase in daily diuresis, an increase in the excretion of glucose, an excretion of protein and creatinine.
PROGRAM ON CONTINUOUS POSTGRADUATE EDUCATION ON NEPHROLOGY
Secondary hyperparathyroidism (sHPT) is a frequently occurring severe complication of advanced kidney disease. Its clinical consequences include extraskeletal vascular and valvular calcifications, changes in bone metabolism resulting in renal osteodystrophy, and an increased risk of cardiovascular morbidity and mortality. Calcimimetics are a cornerstone of parathyroid hormone (PTH)-lowering therapy, as confirmed by the recently updated 2017 Kidney Disease: Improving Global Outcomes chronic kidney disease – mineral and bone disorder clinical practice guidelines. Contrary to calcitriol or other vitamin D-receptor activators, calcimimetics reduce PTH without increasing serum-calcium, phosphorus, or FGF23 levels. Etelcalcetide is a new second-generation calcimimetic that has been approved for the treatment of sHPT in adult hemodialysis patients. Whereas the first-generation calcimimetic cinacalcet is taken orally once daily, etelcalcetide is given intravenously thrice weekly at the end of the hemodialysis session. Apart from improving drug adherence, etelcalcetide has proven to be more effective in lowering PTH when compared to cinacalcet, with an acceptable and comparable safety profile. The hope for better gastrointestinal tolerance with intravenous administration did not come true, as etelcalcetide did not significantly mitigate the adverse gastrointestinal effects associated with cinacalcet. Enhanced adherence and strong reductions in PTH, phosphorus, and FGF23 could set the stage for a future large randomized controlled trial to demonstrate that improved biochemical control of mineral metabolism with etelcalcetide in hemodialysis patients translates into cardiovascular and survival benefits and better healthrelated quality of life.
ISSN 2541-9439 (Online)