LEADING ARTICLE
The kidney is the most important organ for water homeostasis and waste excretion. It performs several important physiological functions for homeostasis: it filters the metabolic waste out of circulation, regulates body fluid balances, and acts as an immune regulator and modulator of cardiovascular physiology. The development of in vitro renal disease models with pluripotent stem cells (both human embryonic stem cells and induced pluripotent stem cells) and the generation of robust protocols for in vitro derivation of renal-specific-like cells from patient induced pluripotent stem cells have just emerged. Here we review major findings in the field of kidney regeneration with a major focus on the development of stepwise protocols for kidney cell production from human pluripotent stem cells and the latest advances in kidney bioengineering (i.e. decellularized kidney scaffolds and bioprinting). The possibility of generating renal-like three-dimensional structures to be recellularized with renal-derived induced pluripotent stem cells may offer new avenues to develop functional kidney grafts on-demand.
REVIEWS AND LECTURES
Endotoxin – obligatory component of gram-negative bacteria cell wall – one of the main etiological factors of chronic inflammation in patients with chronic kidney disease. Endotoxinemia severity increases with the progression of renal failure. The main sources of endotoxin are colon microbiome, as well as the biofilm formed by bacteria in the water treatment system, venous catheters, etc. Endotoxin causes persistent violations of homeostasis: cellular and humoral immunity, metabolic disorders, etc. The correction of these disorders is a complex problem. Endotoxinemia in patients with chronic kidney disease significantly affects the results of treatment and increases mortality.
The review summarizes basic causes and mechanisms of renal allograft rejection, describes the modern concept of immune tolerance formation.
The modern concept of patient’s post-transplantation care is focused on immunosuppression reduction where minimal side effects of these medications is registered and there is no rejection of renal allograft. Photopheresis is one of methods which inspire decrease of allograft rejection and immunotolerance formation.
ORIGINAL ARTICLES. CLINICAL INVESTIGATIONS
THE AIM of the study was to determine the prevalence and severity of mineral and bone metabolism in patients with chronic kidney disease (CKD) undergoing renal transplant. PATIENTS AND METHODS. The study included 77 patients (32 men, 45 women, mean age 44) with CKD who underwent transplantation of cadaveric kidneys from 2011 to 2015. Serum concentrations of electrolytes, the activity of total alkaline phosphatase (ALP), albumin, nitrogen metabolism parameters were determined by standard methods, blood concentrations of parathyroid hormone (PTH) and vitamin D (25-OH vitamin D) – by chemilumescent analysis on ARCHITECT-system. Serum calcium on serum albumin is reassessed, glomerular filtration rate (GFR) is calculated according to the formula CKD-EPI. RESULTS. Hypercalcemia, hypophosphatemia, hypomagnesemia and a high level of PTH respectively diagnosed in 15.6%, 16.9%, 16.9% and 87% patients. There was the high significant difference between blood PTH in patients with normal renal function and reduced renal graft function. The blood level of vitamin D ranged from 6 to 30 ng/ mL (median 14), only one patient was in a recommended range (≥30 ng/ml). There was the invert correlation of PTH with GFR (r=-0.543, p<0.001) and serum magnesium (r=-0.241, p=0.04), directl correlation with total ALP activity (r=0.280, p=0.015). The blood PTH is not associated with serum calcium and phosphorus. There was weak invert correlation between serum phosphorus and GFR (r=-0.232, p=0.04), between ALP activity and GFR (r =-0.267, p=0.02) and between serum magnesium and GFR (r=-0.230, p=0.05). CONCLUSION. Common manifestations of mineral and bone disorders in renal transplant recipients are pre- and post-transplantation hyperparathyroidism, which development/progression is associated with hypomagnesemia, deterioration of kidney function, as well as deficiency of vitamin D.
THE AIM: is to analyze the histological results of the method extracorporeal photochemotherapy in cadaveric kidney allotransplantation. PATIENTS AND METHODS. Extracorporeal photochemotherapy has been used as a prevention of acute renal allograft rejection in the early postoperative period in 20 patients. The control group consisted of 20 patients with paired to basic group transplants without using of this method. Patients in both groups carried out the transplant protocol biopsies at 30 and 180 days after transplantation or when indicated, followed by the conclusion of histological classification according to the Banff 2007. Also showed a clinical case of the use of extracorporeal photochemotherapy as a therapy of transplant glomerulonephritis. RESULTS. It was established that in the basic group biopsy did not show any evidence of the transplant rejection, at the same time in 4 patients in comparison group histology confirmed rejection of the transplanted organ varying degrees of Banff 2007, two of which have resulted ingraft loss. Applications of extracorporeal photochemotherapy as the treatment of transplant glomerulonephritis showed that the method can be used to normalize graft function and is able to stop the development of focal and segmental glomerulosclerosis, that was confirmed by histological examination of a biopsy sample before and after treatment. CONCLUSION. Extracorporeal photochemotherapy is effective and can be used as adjuvant therapy for the prevention of renal allograft rejection and as a therapy of returned transplant glomerulonephritis.
AIM – to evaluate efficiency of use of combined human intravenous immunoglobulin (IVIG) with plasmapheresis and rituximab for transplantation glomerulopathy in late period after kidney transplantation. PATIENTS AND METHODS. The study included 50 patients with morphologically verified transplantation glomerulopathy, 24 of which received plasmapheresis with IVIG and rituximab. Control group consisted of 26 patients without antihumoral treatment. RESULTS. At diagnosis GFR in study and control groups has no differ (44.9 Ѓ} 21.3 vs 41.2 Ѓ} 14.6 ml/min, P =0.47), but following graft function depression rate was lower in group which received treatment in comparison with control group: -0.47 Ѓ} 0.6 ml/min/month и -1.31Ѓ} 1.6 ml/min/month (p = 0.02). Therefore 3-year survivability of graft was 21.3% vs 64.8% in patients receiving treatment (Р=0,01). CONCLUSION. Our study showed that transplantation glomerulopathy as the most often variant of chronic humoral rejection is characterized by unfavorable prognosis regardless of its morphological case and process activity at diagnosis. Combined treatment including plasmapheresis, human intravenous immunoglobulin and rituximab makes it possible to delaythe progression of chronic rejection at least in some patients with chronic humoral rejection revealed in late period after renal allotransplantation.
THE AIM: to estimate an influence of plasmapheresis (PA), carried in early postoperative period, on 15-year results of renal transplantation. PATIENTS AND METHODS. In 32 children operated at 1995-1996 years PA was not carried. This group was called “before PA”. In 32 children, operated at 1996-1997 years, PA was carried in early postoperative period. This group was called “PA”. In 31 patients operated at 1997-1998 years, PA was not carried, but their inductive immunosuppression was intensified with ATG, introduction of cyclosporine microemulsion and CellSept. This group was called “after PA”. RESULTS. Actuarial survival of both patients and grafts was highest in group “PA” and “after PA” compared to other groups. The difference was statistically significant. CONCLUSION: plasmapheresis done in the early posttransplant period may have a positive influence on long-term outcomes o f kidney transplantation in children.
THE STUDY was aimed to define the incidence rate and outcomes of antibody-mediated rejection (AMR) in the routine morphological and immunological monitoring. PATIENTS AND METHODS. 55 recipients of kidney allograft (KA) were enrolled into the study according to inclusion criteria (AB0-compatibility, negative cytotoxic crossmatch, minimum 3 kidnеy allograft biopsies in posttransplant period). All patients were on standard immunosuppressive regimen: glucocorticosteroids, basiliximab, calcineurin inhibitors, mycophenolate mofetil. Protocol (on 3, 6, 12 months and then annually) and indicative (delayed graft function, increase of serum creatinine level of ≥25%, proteinuria ≥1 g/24h) KA biopsies were evaluated according to Banff classification 2013. Enzyme-linked immunosorbent and multiplex (Luminex; xMAP Technology) assays were applied for donor-specific antibodies screening and monitoring, respectively. The treatment of AMR included glucocorticosteroids, plasma exchange, intravenous immunoglobulin, rituximab, bortesomib. KA loss and return to dialysis were defined as an outcome. Long-term KA prognosis was estimated by Kaplan–Meier survival analysis. The median posttransplant follow-up was 65 (47; 80) months. RESULTS. Morphological features of AMR was established in 13% of biopsies (n=390) and 45% of patients met Banff 2013 AMR criteria. Acute AMR (aAMR) and chronic active (cAMR) were found in 13 and 12 KA recipients, respectively. 48% of cases showed subclinical type of AMR. Persistence and chronification of AMR were established in 56% and 77% of patients, respectively. Cumulative 9-year patient survival in the group studied (n=55) for the follow-up period was 94,5%, cumulative survival of KA was 79%. KA survival was worse in AMR patients when compared with the control group without AMR (73% vs 100%, plog-rank=0,016). There were no difference in KA survival in aAMR and cAMR as far as in clinical and subclinical types of AMR. CONCLUSION: AMR is supposed to be the frequent and under-recognized clinical problem associated with inferior KA survival and overall effectiveness of kidney allotransplantation. The approach to early diagnostic and treatment of this type of immune conflict requires the immunological and morphological monitoring of КА on a regular basis.
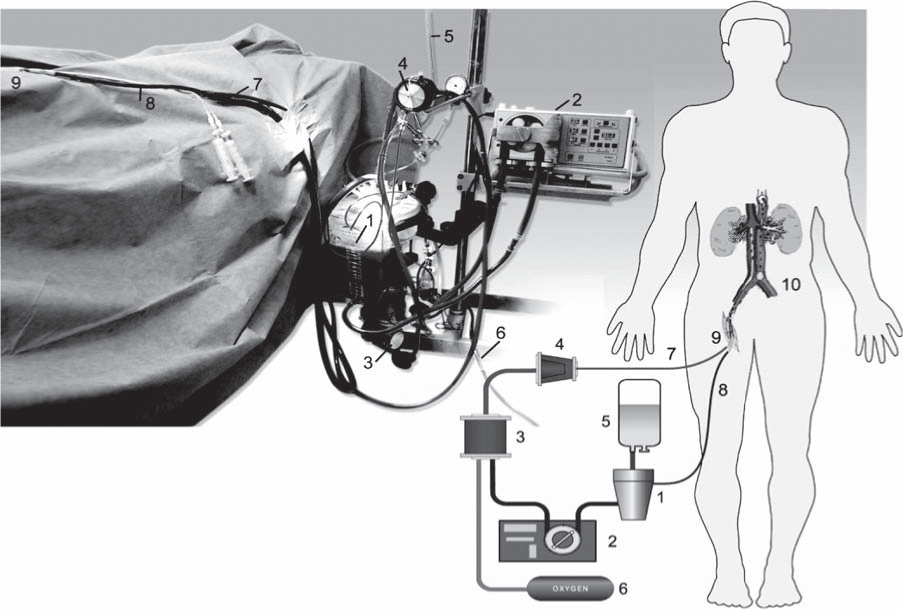
THE AIM. To offer procurement society reliable protocol of full kidney transplants from donors with heart death based on 5-year results of kidney transplants received via protocol normothermic hemoperfusion with extracorporeal oxygenation. PATIENTS AND METHODS. The study included 29 DCD kidneys (primary warm ischemic time – 58,1 (19,39) minutes), received with use of suggested protocol and estimated results of such grafts transplantation to 58 recipients. Received data were validated by comparison with outcomes of 112 kidney transplantations from 115 brain death donors (BDDs). RESULTS. In study group IGF was observed in 28 (48.3%) of the 58 recipients, in control group – 63,4% (71 recipient). There were 4 cases of PNFT, these patients were not included into study group. The actuarial 5-year graft survival rate was 82,8% (n=48) as contrasted with 87,5% (n=98) (BDDs) (p>0,05). Serum creatinine levels over 5 years after transplantation were 0,094(0,06)mmol/l in recipients of DCD kidneys and 0,103(0,07)mmol/l – BDD kidneys (p>0,05). CONCLUSION. Reconstruction and survival of procurement organs from unexpectedly died persons with critical asystole period with extracorporeal perfusion in situ is promising protocol. Use of thrombolytics and mechanical perfused removal of leukothromboagglomerates formed during lack of blood circulation are necessary. The 5-years outcomes of kidney transplantation received from DCD with use of extracorporeal perfusion in situ did not differ from outcomes of kidney transplantation from BDDs.
PRACTICAL NOTES
Chronic lymphocytic leukemia (CLL) is the most frequent form of leukemia inWestern Europe. Despite of high frequency of this type of leukemia, kidney involvement associated with CLL is rarely reported in the literature. Renal biopsies are not routinely performed in patients with CLL to evaluate unexplained renal insufficiency or nephrotic syndrome (NS). As a consequence, little is known about mechanisms causing renal abnormalities in CLL. Collectively, 130 cases of biopsy-proven glomerular or interstitial renal abnormalities due to CLL have been reported in the literature to date. The most common type of glomerulonephritis causing NS during CLL is membranoproliferative glomerulonephritis, less frequent causes include membranous nephropathy, minimal-change disease. Focal segmental glomerulosclerosis (FSGS) is a rarity; we met only 6 observations of FSGS associated with CLL that have been published to date. We present a rare case of CLL-associated FSGS with clinical resolution of the NS after successful treatment with rituximab and literature review on various nephrotic glomerulonephropathies associated with CLL manifestative with NS.
PROGRAM ON CONTINUOUS POSTGRADUATE EDUCATION ON NEPHROLOGY
Kidney transplantation (KT) until recent time was considered contraindicated to patients with end stage kidney failure due to atypical hemolytic uremic syndrome (aHUS) because of high risk of recurrence of the underlying disease and graft loss. However, it has now developed new approaches to prevention and treatment aHUS relapse in posttransplantation period, which significantly improved KT results in these patients. This article discusses the principles of risk assessment aHUS relapse after transplantation, the donor organ selection, features of immunosuppressive therapy, prevention and treatment of aHUS episodes in renal transplant recipients.
ANNIVERSARIES
INDEXES
ISSN 2541-9439 (Online)